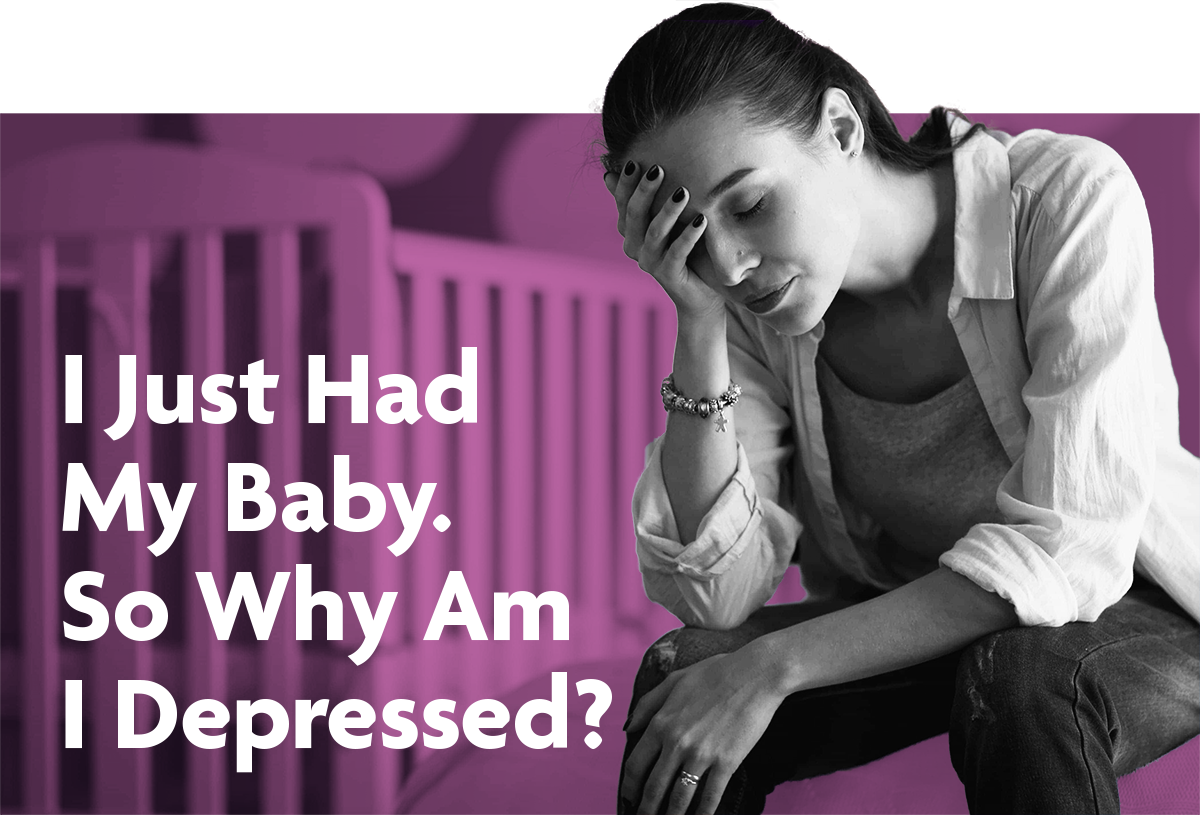
I Just Had My Baby.
So Why Am I Depressed?
Learn the facts about postpartum depression.
Schedule an Appointment559-664-4000
What Is Postpartum Depression (PPD)?
Mothers with postpartum depression experience intense, long-lasting feelings of sadness, anxiety, or despair that prevent them from completing their daily tasks and routines. In mothers, PPD is often caused by a combination of factors, including:
- Sharp post-pregnancy changes in hormone levels.
- A history of depression.
- Fatigue and stress.
- Other lifestyle and emotional factors.
It’s okay to ask questions about mental health after you’ve had your baby. Here are some common questions many mothers ask about postpartum depression:
About half of new mothers experience a mild depression after giving birth – an experience known as the baby blues (postpartum blues). Baby blues symptoms include:
- Mood swings.
- Anxiety.
- Sadness.
- Irritability and anger.
- Crying (often for no reason).
- Trouble sleeping, eating, and making choices.
Most often, the baby blues dissipate one to two weeks after a mother gives birth. However, some mothers (10 to 20 percent) find that these feelings don’t fade. Instead, they intensify.
This is the start of postpartum depression (PPD). PPD symptoms include:
- Depression.
- Excessive crying.
- Difficulty bonding with your child.
- Withdrawl from family and friends.
- Sudden or drastic changes to sleep schedule and appetite.
- Intense irritability and anger.
- Feelings of worthlessness, shame, or guilt.
- Restlessness, severe anxiety, and panic attacks.
- Thoughts of harming your child or yourself.
If you find yourself experiencing these symptoms any time after giving birth, you should see your healthcare provider as soon as possible.
Postpartum depression DOES NOT always occur directly after giving birth. It can occur any time up to one year after you’ve had your baby, though it most commonly starts one to three weeks after birth.
You absolutely can treat postpartum depression – and you should schedule an appointment with your healthcare provider as soon as you (or a friend or loved one) suspect you might have PPD.
While the exact treatment depends on the nature and severity of your depression, it might include:
- Counseling.
- Support groups.
- Talk therapy.
- Medication.
You CAN take antidepressants while breastfeeding, though you should consult your provider about the potential risks and usage.
You are not a bad mother, and you are not alone. Ten to twenty percent of mothers experience some form of PPD. With help, the symptoms are manageable. Mothers with PPD can care for their children just as well as those without – but you should be willing to seek help.
Postpartum anxiety affects roughly 10 percent of new mothers. It includes symptoms such as:
- Changes in your eating and sleeping schedule.
- Constant worry, fear, and racing thoughts.
- Trouble focusing and sitting still.
- Physical symptoms such as dizziness, hot flashes, and nausea.
However, postpartum anxiety is NOT the same as postpartum depression. You can experience one, the other, or both at the same time. Additionally, postpartum anxiety can extend as far as experiencing panic attacks or temporary symptoms of obsessive-compulsive disorder.
If you experience any of the above symptoms during or after your pregnancy, schedule an appointment with your provider immediately. Postpartum anxiety is treatable, as long as you make your provider aware of your symptoms.
I Think My Friend, Loved One, or Partner Might Have PPD. How Do I Help Them?

First, encourage them to talk to you about their current emotional state. They may not recognize or acknowledge that they’re depressed, and may be hesitant to talk about their feelings. Regardless, sit them down for an honest conversation.

Then, recommend they schedule an appointment with their healthcare provider (or schedule one for them). Make sure they keep the appointment. Getting professional help, immediately, is key to managing PPD.
What Should I Do Next?
If you suspect that you or someone you love has PPD, have that person schedule an appointment immediately.
Remember, You Are Not Alone
Start the conversation. To speak with a Behavioral Health Specialist, please fill out the below form.
Camarena Health – 559-664-4000
For Emergencies Contact 911 or the National Crisis Line 800-273-8255